Introduction
Myelomeningocele is a type of spina bifida (SB) which is the second most common SB abnormality that occurs in developing babies. In this birth defect, meninges (covering membranes of the Central Nervous System or CNS) protrude from the back of child along with the spinal cord or cauda equina due to a neural tube defect. Cauda equina are the descending nerve roots from the lowest part of the spinal cord. This congenital abnormality can be prevented by adding folic acid supplements to the diet during pregnancy. Early diagnosis also helps treating this birth defect. The solution to myelomeningocele is a special surgical procedure. This article discusses the importance of surgery for myelomeningocele along with other important steps.
Intensive Care
Myelomeningocele is birth defect with serious complications. So, the patient with myelomeningocele needs intensive management by the specialists. The patients with this abnormality may present with the following complications:
• Hydrocephalus is an abnormal condition of the brain where fluid accumulates in the chambers or cavities of the brain and exerts pressure on the adjacent structures. It is present in 80-90% of cases of myelomeningocele. Cerebrospinal fluid (CSF) is fluid that washes the brain and spinal cord to protect their tissues. Normally, CSF is produced by the brain tissues. It baths the central nervous system (CNS) and then is drained out. But, in the case of hydrocephalus, the drainage system for CSF gets damaged. So, CSF accumulates in the surrounding of CNS and ventricles (cavities) of brain. In this condition CSF puts pressure on the tissues of central nervous system that can cause damage. In order to drain CSF, shunting is performed. During the surgical procedure of shunting, a tube is placed between the ventricles of brain and abdomen. It is also called ventriculoperitoneal shunting. Another type of shunting is called ventriculoatrial shunting where a tube is placed between ventricles of the brain and a chamber of the heart called the atrium.
• Chiari syndrome is a condition which affects the balance and coordination. It may also be present with cases of myelomeningocele. The patient may present with difficulty in breathing, slow heart rate and swallowing problems.
• Latex allergy is most commonly seen in the patients with myelomeningocele. As the child undergoes many surgical procedures during early childhood the use of latex gloves may cause a latex allergy. Latex allergy is more common in these patients than in normal ones. So, the use of latex gloves should be avoided.
• Bowel/bladder functioning is monitored regularly and urologists are also consulted as nerves of these areas are prone to be damaged.
• Cognition and intelligence may or may not be affected in these patients because some children with myelomeningocele history show normal or greater than normal intelligence. Cognitive functions are affected due to hydrocephalus. But, if hydrocephalus is treated in time, this damage can be prevented.
• Physical balance and strength can be affected. These functions can be improved by physiometric assessments. Walking and muscular movements of legs can be affected due to the involvement of the nerves. Intensive physiotherapy for these patients by specialists can make some improvements.
Surgical Procedure
A child affected with meyelomeningocele is treated by surgically closing the opening present on child’s back. This is a surgical procedure that is performed in one of the two ways: when the baby is in the mother’s womb (pre-natal) or when the baby has been delivered (post-natal).
• The pre-natal procedure is still under evaluation and is performed in a few hospitals in America. It is performed during pregnancy when the condition is diagnosed before 25 weeks of gestation. It cannot be performed in every woman because there can be some complications. In this procedure, the opening of myelomeningocele is closed in the uterus by cesarean section (a surgical procedure to deliver baby).
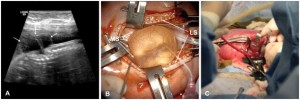
• The post-natal procedure is performed within 24 to 48 hours after delivery to avoid further damage to the CNS and risk of infection due to exposure of the spinal cord and its coverings to the external environment. Before the surgery, the back is covered by a sterile dressing and the patient is kept lying on their side to avoid pressure on the nerves and spinal cord. In case of breach, there may be some changes in procedure. The area is carefully cleansed with saline. Figure 1 shows the surgical procedure images.
Figure 1: Pre-natal surgical procedure to treat myelomeningocele (Source: www.ncbi.nlm.nih)
Importance of surgery
Surgery is the best treatment for myelomeningocele. As mentioned before, it can be performed pre-natally as well as post-natally. There are some advantages of the pre-natal surgery over the post-natal surgery; however, pre-natal surgery is still in trail. Table 1 compares the outcomes of a randomized trial of 183 women for these two choices in surgery. There is some indication that the pre-natal surgery is more beneficial in the child’ s motor development.
Table 1: Management of myelomeningocele by pre-natal and post-natal surgery. (Source: www.acog.org)
The importance of pre-natal surgery is as follows:
- By pre-natal surgery, damage to the spinal cord and nerves can be minimized by covering the exposed area of back. Damage to the exposed area of central nervous system may be increased due to infection if pre-natal surgery is not performed. But pre-natal surgery is very critical procedure requiring intensive care treatment of the mother and fetus. A neurologist, orthopedic specialist and urologist are consulted whenever such surgery is planned.
- In post-natal surgery, the exposed area of the spinal cord and meninges is covered with a non-latex sterile dressing after birth. The patient may be allergic to latex, so non-latex gloves are used during surgery. After surgery, further steps are taken to improve the healthy life of the child. The patient needs to visit specialists for a year to consult about the function of bowel/bladder, muscles of legs and cognition.
If surgery is not carried out in time, the patient’s condition may deteriorate. Problems with the bladder, bowel and muscles may increase. The exposed area is always at risk of infections which may increase the damage to nerves and spinal cord tissue, thus affecting their functioning ability. The patient may get paralyzed and disabled completely.
Counseling
Families having a child with myelomeningocele are facing a critical time. So, they should be counseled by pediatric neurologists, urologists and specialists helping their child. By counseling, they receive much information about this birth defect that will help them in making decisions about the future of the child. The parents will make their choice about abortion, adoption, pre-natal or post-natal surgery or whatever is needed.
Reference
Kinsman SL, Johnston MV. Congenital anomalies of the central nervous system. In: Kliegman RM, Behrman RE, Jenson HB, Stanton BF, eds. Nelson Textbook of Pediatrics. 18th ed. Philadelphia, Pa: Saunders Elsevier; 2007:chap 592.
Adzick NS, Thom EA, Spong CY, Brock JW 3rd, Burrows PK, Johnson MP, et al. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med 2011;364:993–1004.
Johnson MP, Sutton LN, Rintoul N, et al. Fetal myelomeningocele repair: short-term clinical outcomes. Am J Obstet Gynecol 2003; 189:482.
Sutton LN. Fetal surgery for neural tube defects. Best Pract Res Clin Obstet Gynaecol 2008; 22:175.
Chen CP. Prenatal diagnosis, fetal surgery, recurrence risk and differential diagnosis of neural tube defects. Taiwan J Obstet Gynecol 2008; 47:283.