Introduction
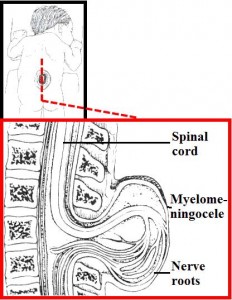
Lumbar myelomeningocele is one of the types of spina bifida, a defective closure of the vertebral column. A myelomenigocele refers to a protrusion of the covering membranes of the spinal cord (meninges) due to a defect in the spinal canal during the development of baby (early fetal stage). The spinal canal is a long vertical cavity where spinal cord lies. In some instances the protrusion of meninges may result from the reopening of the tube as a result of an abnormal increase in cerebrospinal fluid (CSF: fluid which baths the central nervous system) pressure. Spinal coverings are not completely covered by skin and thus the thin meninges may rupture a few days after birth.
Figure 1: Lumbar Myelomeningocele (Source: www.neuros.net)
Signs & Symptoms
Lumbar myelomeningocele can be diagnosed at birth as well as during pregnancy. In any patient with myelomeningocele who presents with mental, bony, urinary problems, possible uncontrolled hydrocephalus (abnormal accumulation of CSF) should be excluded to reach the final diagnosis before any treatment is pursued, including the following symptoms:
- Laryngeal and pharyngeal paralysis
- Shortness of breath
- Difficulty in swallowing
- Harsh sounds during respiration
- Nystagmus (involuntary and rapid movements of eyeball)
- Upper extremity weakness
- Co-ordination difficulty
- Cognitive function- intelligence, thought and problem-solving ability)
- Tethered spinal cord
Sometimes a stretched spinal cord in the spinal canal can be indicated by foot deformities, new onset of hip dislocation or worsening of the spinal deformity. Progressive neurologic defects in growing children may suggest a lack of extensibility of the spine or indicate that the spine is malformed or tethered and low-lying in the spinal canal of the flank, with the potential for progressive, irreversible neurologic damage requiring surgical repair.
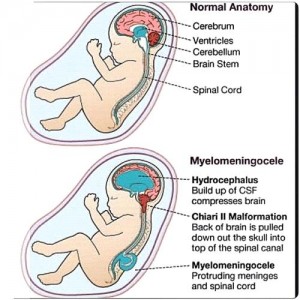
Sometimes, a condition called Chiari type II malformation may cause acute signs and symptoms as the lower part of the brain and upper part of cervical spinal cord undergo compression. See Figure 2.
Figure 2: Fetal normal anatomy and myelomeningocele (Source: www.media.tumblr.com )
Epidemiology
Worldwide 1 to 2 cases of spina bifida per 1000 of population are reported and its occurrence depends mostly on the genetics. Folic acid supplements have decreased its rate, along with early diagnosis and improved nutrition among pregnant women. Spina bifida occurs 1 to 2 cases per thousand but it differs from area to area. The frequency of neural tube defects (birth per 10,000), is 0.9 in Canada and 11.7 in America??. These incidence levels also occur differently among white and black, but occur more in the white population. Hispanics have a high incidence.
Laboratory Diagnosis
Laboratory screening tests for neural tube defects can be performed and this is done by the following methods:
- Elevated alpha-fetoprotein (AFP: a protein produced by fetal liver, yolk sac and intestines) level in amniotic fluid is marked as a neural tube defect. Peak concentrations of AFP in the 13th to 15th weeks of pregnancy permit diagnosis.
- To check the functioning of kidneys, urine analysis is done, likewise monitoring urea and creatinine level in the serum.
- Fetal ultrasonography is thought to be the basic screening test for babies with neural tube defects, usually done at approximately 18 weeks gestational age.
- Radiographs of the vertebrae provide information for early evaluation when an infant is born with myelomeningocele.
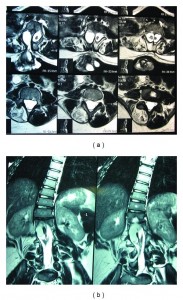
- Hydrocephalus (resulting from a buildup of fluid in the brain) can be detected with serial ultrasonograms of the skull in infants and computed tomography (CT) scans or magnetic resonance imaging (MRI) of the spine and brain in adults.
- A patient with hydrocephalus is prone to brain damage and his/her intelligence and cognitive functioning become impaired. In this condition, psychological treatment is recommended.
- By body movements and gait, a patient’s ability to co-ordinate muscle movements can be monitored.
Figure 3: (a). Axial lumbar MRI T-2 images demonstrating a type 1 split cord malformation with the myelomeningocele attached to the right hemicord. (b). Coronal lumbar MRI T-2 images demonstrating a type 1 split cord malformation with a neurenteric cyst attached to the right hemicord (Source: ncbi.nlm.nih.gov).
Treatment
The following are approaches for the treatment of myelomeningocele:
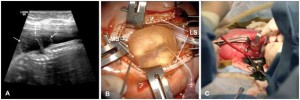
Surgery: Closure of the myelomeningocele is performed by surgery immediately after birth. Steps in the closure procedure include extensive undermining of the skin, dissection of the neural mass that is replaced into the spinal canal, and watertight closure of the duramater (a covering of spinal cord) and layers of skin. A neurosurgeon is also required to monitor along with other operating room staff. In addition, urologic evaluation is necessary to establish medication to prevent frequent urologic infections that occur with SB.
Figure 4: Large lumbar myelomeningocele
Catheterization for bladder: In this procedure, a tubular instrument is passed through body channels to drain fluid. Intermittent catheterization and vesicostomy (incision into the bladder to divert flow of urine when the bladder can no longer function) are used to drain the bladder. Catheterization on regular time schedule keeps children drier, less prone to infection and in better control of urinary function.
Physical Therapy: While treating newborns with myelomeningocele, the physical therapist offers muscle function improvement. In this way, joint alignment, muscle imbalance, contractures, posture, and signs of progressive neurologic dysfunction can be monitored.
Shunting for hydrocephalus: In 80-90% of children with this disability there is the need to find a way to drain CSF. This process is called shunting. Basically a drainage tube is run from the brain ventricles to a cavity in the abdomen or even the heart. Other techniques include ventriculoatrial (surgical communication between cerebral ventricles and cardiac atrium by tube) and ventriculopleural shunting (communication between cerebral ventricle and peritoneum by tube) .
Medications: Medications used most frequently in myelomeningocele are for treatment of bladder dysfunction caused by damaged nerves. These medications are used in conjunction with some form of bladder emptying techniques to prevent upper urinary tract complications and to facilitate social continence. Among the drugs used are the following:
- Anticholinergics: oxybutynin chloride, hyoscyamine sulfate
- Tricyclic antidepressants: imipramine hydrochloride; may act through anticholinergic effects
- Alpha-adrenergic antagonists: terazosin
Prevention
The reduced incidence of myelomeningocele is due to the increasing availability and accuracy of the tests which are done before delivery to diagnose the congenital disorders. There is the option for early pregnancy termination and the introduction of primary prevention in the form of folic acid therapy before and during pregnancy. The US Preventive Services Task Force recommends 400-800 mcg of folic acid every day. However, the metabolism of folic acid appears to be abnormal in affected patients, suggesting that spina bifida may result from an inherited defect rather than strictly from a deficiency.
Reference
Danzer E, Gerdes M, Bebbington MW, et al. Preschool neurodevelopmental outcome of children following fetal myelomeningocele closure. Am J Obstet Gynecol 2010; 202:450.e1.
Tomita T, McLone DG. Acute respiratory arrest. A complication of malformation of the shunt in children with myelomeningocele and Arnold-Chiari malformation. Am J Dis Child 1983; 137:142.
Holinger PC, Holinger LD, Reichert TJ, Holinger PH. Respiratory obstruction and apnea in infants with bilateral abductor vocal cord paralysis, meningomyelocele, hydrocephalus, and Arnold-Chiari malformation. J Pediatr 1978; 92:368.
McLone DG, Dias MS. The Chiari II malformation: cause and impact. Childs Nerv Syst 2003; 19:540.
McLone DG, Knepper PA. The cause of Chiari II malformation: a unified theory. Pediatr Neurosci 1989; 15:1.
Naidich TP, McLone DG, Fulling KH. The Chiari II malformation: Part IV. The hindbrain deformity. Neuroradiology 1983; 25:179.
Harmon JP, Hiett AK, Palmer CG, Golichowski AM. Prenatal ultrasound detection of isolated neural tube defects: is cytogenetic evaluation warranted? Obstet Gynecol 1995; 86:595.
Centers for Disease Control and Prevention (CDC). Racial/ethnic differences in the birth prevalence of spina bifida – United States, 1995-2005. MMWR Morb Mortal Wkly Rep 2009; 57:1409.
Frey L, Hauser WA. Epidemiology of neural tube defects. Epilepsia 2003; 44 Suppl 3:4.
Adzick NS, Sutton LN, Crombleholme TM, Flake AW. Successful fetal surgery for spina bifida. Lancet 1998; 352:1675.
Chen CP. Prenatal diagnosis, fetal surgery, recurrence risk and differential diagnosis of neural tube defects. Taiwan J Obstet Gynecol 2008; 47:283.
Sutton LN. Fetal surgery for neural tube defects. Best Pract Res Clin Obstet Gynaecol 2008; 22:175.
Johnson MP, Sutton LN, Rintoul N, et al. Fetal myelomeningocele repair: short-term clinical outcomes. Am J Obstet Gynecol 2003; 189:482.