2 Types of Prenatal & Postnatal Myelomeningocele Treatment Options
Myelomeningocele is type of spina bifida, characterized by herniation of spinal cord contents and meninges through an abnormal defect in the vertebral column [1].The exact cause is still not known but there are certain factors which are considered to be associated with the occurrence of it. These factors may result in defective closure of the lower end of the neural tube during early fetal development. Though it may be located anywhere along the spinal cord the lumbosacral area is the most common location. Depending upon the location, it can be classified into various types, such as, thoracic, lumber, sacral, anterior, posterior and lateral myelomeningocele [2,3].
Myelomeningocele is the most common type of spina bifida affecting as many as 1 out of every 800 babies [2]. It can also be detected before the delivery of the baby. Prenatal screening tests for the detection of it include serum alpha fetoprotein (AFP) levels, quadruple/triple screen, ultrasonography and amniocentesis. A patient with this condition presents various clinical features, such as, difficulty in walking, poor coordination in walking, paralysis of lower limbs, numbness of lower limbs, pain and heaviness in lower limbs, urinary frequency, urgency and incontinence, constipation and hydrocephalus [5].
Myelomeningocele Treatment Options
Myelomeningocele treatment can be carried out at two times: prenatal and postnatal.
Prenatal myelomeningocele options
Various surgical procedures for fetuses using animal models were first developed at the University of California, Sans Francisco in 1980 by Dr. Michael and his colleagues. Fetal Myelomeningocele Treatment refers to a prenatal surgical treatment that includes a wide range of surgical procedures that are performed to treat these birth defects in fetuses which are still in the uterus. Open fetal surgical treatment refers to complete opening of the abdomen and uterus to operate on the developing fetus. Minimally invasive fetoscope operation (fetal Myelomeningocele Treatment) is performed on fetuses by using small incisions, fetoscope and sonography [6].
Various prenatal fetal Myelomeningocele surgeries
Open Fetal Myelomeningocele Treatment
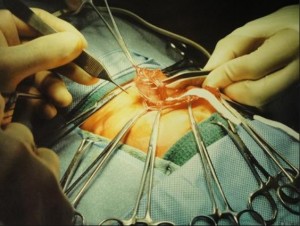
This treatment of myelomeningocele is an complete incision that is made in the abdomen and the uterus to operate on the fetus. It includes the following steps:
Certain drugs called as tocolytics are generally administrated to the pregnant woman to prevent labor. However, these drugs should not be avoided in the presence of intrauterine infection, unexplained vaginal bleeding and fetal distress. A drug which reduces stomach acid secretion (like H2-antagonists) is usually given the evening before and the morning of the surgical treatment, and an antacid like magnesium bicarbonate is usually administrated before induction to avoid the risk of acid aspiration. For sedation and intubation, a rapid sequence induction is used.
To review, the following steps are performed during this operation:
- Administrating the tocolytics to avoid labor
- Administrating H2-antagonists and antacids a day before the procedure to reduce the chances of acid aspiration
- Rapid sequence induction for sedation and intubation
- Opening the uterus by incision, called an hystertomy
- Exposing the fetus
- Performing surgical procedures on the fetus to correct or repair spina bifida
- Returning the fetus to the uterus
- Closing the uterus and abdominal wall
- Before applying the last stitch in the uterine wall, the amniotic fluid is replaced
After the operation, the woman stays in the hospital for 3–7 days for post-operative monitoring and care. Later a cesarean section is performed to deliver the baby. The baby thus delivered may be preterm. The exact time of performing this operation ranges between 18-30 weeks of gestation [7].
Minimally invasive fetal surgerical
Minimally invasive fetal Myelomeningocele Treatment is performed via very small incisions under the guidance of real-time video imagery from fetoscopy and ultrasonography [8].
Postnatal Myelomeningocele treatment options
Surgical repair is the most common choice of treatment of myelomeningocele after birth. The baby must be handled carefully before the surgical repair to avoid the chances of spinal cord injury. It is very important to perform a surgical repair to close the defect within the first 48 hours after delivery to preserve neural tissue and to prevent other complications, such as, infections. A shunt can be placed in case of hydrocephalus during or after the operation. Antibiotics are given to the baby as a prophylaxis to prevent infections.
The Boston Children’s hospital talks about a controlled study that focuses on prenatal Myelomeningocele treatment options
Postnatal follow up
Some children may acquire a permanent neurological deficit and they may require conservative medical care for their whole life. The different types of medical care may include:
- Care of bowels and urinary bladder with the help of bladder and bowel exercises
- Urinary catheterization in case of urinary retention
- Regular physiotherapy to prevent contractures
- Support from a psychotherapist and social support groups. Sometimes, attendants of the patients with neural tube defects (NTDs) also need social and psychological support.
- Avoidance of latex materials
- Prophylactic use of antibiotics to prevent infections [9].
Conclusion
Myelomeningocele is the most severe form of spina bifida which can be detected prenatally by simple screening tests. Surgical repair is the treatment of choice for it. Prenatal fetal surgery has a better outcome than postnatal surgical repair or management. Some children with permanent neurological deficits may require lifelong conservative treatment.
References
- Myelomeningocele [Internet]. [Last updated 15 Mar 2004; Cited on 30 Oct 2013]. Available from: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0002525/.
- Ahrens K, Yazdy MM, Mitchell AA, Wereler MM. Folic acid intake and spina bifida in the era of dietary folic acid fortification. Epidemiology 2011;22(5):731-7.
- Greene ND, Coppa AJ. Development of the vertebrate central nervous system: formation of the neural tube. Prenat Diagn 2009;29(4):303-11.
- Saboval L,Horn F, Drdulova T, et al. [Clinical condition of patients with neural tube defects]. Rozhl Chir 2010;89(8):471-7.
- Birnbacher R, Messerschmidt AM, Pollak AP. Diagnosis and prevention of neural tube defects. Curr Opin Urol 2002;12(6):461-4.
- Deprest JA, Devlieger R, Srisupundit K, et al. Fetal surgery is a clinical reality. Semen Fetal Neonatal Med. 2010;15(1):58-67.
- Kitano Y, Flake AW, Crombleholme TM, et al. Open fetal surgery for life-threatening fetal malformations. Semin Perinatol. 1999 Dec;23(6):448-61.
- Bui TH, Deprest JA, Ville Y, Westgren M.Minimally invasive techniques make fetal surgery possible. Disabling abnormalities can be corrected. Lakartidningen. 1998;95(44):4848-50, 4853-4.
- Thompson DN. Postnatal management and outcome for neural tube defects including spina bifida and encephalocoeles. Prenat Diagn. 2009 Apr;29(4):412-9.


